While Covid-19 vaccination programs around the world are still in the early stages, it is clear that faith in the vaccines is not globally uniform. Trust is a fragile commodity, and vaccines have been politicized in many countries. Governments, therefore, must take building confidence seriously and deploy significant political will and skill alongside science and facts to strengthen it. Dr Khor Swee Kheng of Chatham House and the United Nations University-International Institute for Global Health writes that these efforts must be pragmatic (through a suite of targeted solutions), holistic (with governments leading all-of-society approaches domestically and internationally), and sustainable (because vaccine confidence is always a moving goalpost).
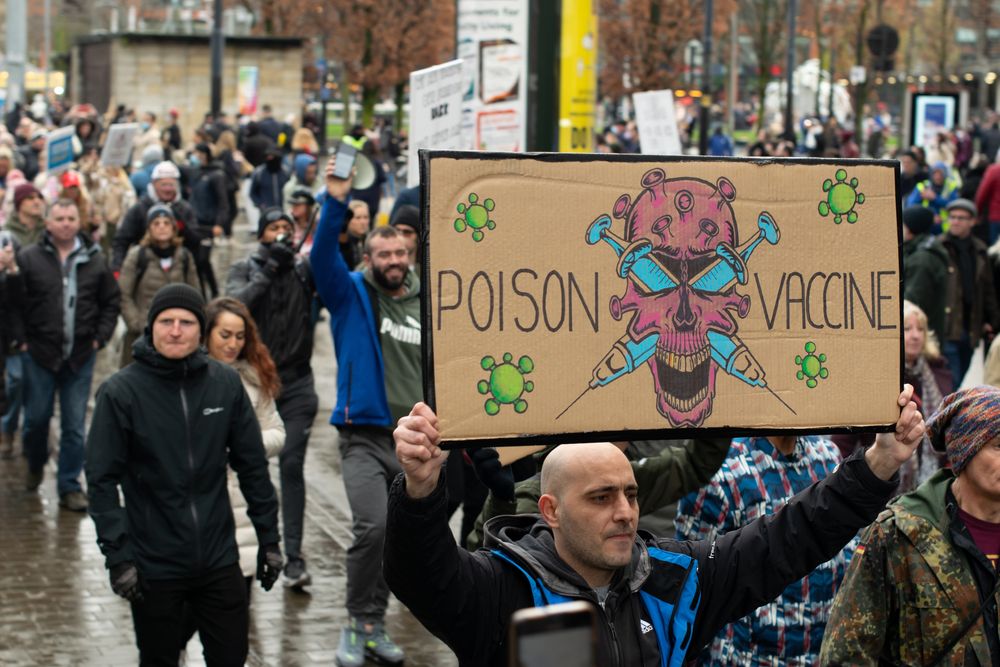
Anti-vaccine protest in Manchester, UK, December 2020: Governments need an all-of-society sustained effort to counter hesitancy (Credit: John B Hewitt / Shutterstock.com)
At first sight, confidence in the Covid-19 vaccine appears high. After all, more than 635 million people worldwide have been vaccinated since public programs started in December 2020. Vaccinations could be even faster if supplies keep up with the strong demand for 14 billion doses before the end of 2021. Even an Imperial College/YouGov survey in February 2021 shows that people worldwide are more and more willing to be vaccinated. These facts suggest that fears of vaccine hesitancy could be misplaced.
Unfortunately, the reality is not as rosy. Even before Covid-19, the World Health Organization (WHO) already labelled vaccine hesitancy as one of the top ten threats to global health, and added the term “infodemic” during the Covid-19 pandemic. Vaccine confidence also depends on many structural and non-scientific factors that often undermine it.
Vaccine confidence is fragile
Only a few months into the first vaccine rollouts around the world, these are key lessons gleaned so far:
First, vaccine confidence is not uniform across the world. There are pockets of hesitation, such as France (which convened a 35-member “citizens’ vaccine panel” to build trust), Japan (which has only vaccinated a paltry 0.7 percent of its population as of 2 April, versus 60.7 percent in Israel and 30.4 percent in the United States), and the Philippines (where social-media rumors after the 2016 dengue vaccine controversy turbo-charged vaccine hesitancy). If not adequately addressed, reluctance to get inoculated could deepen in these countries or even spread more broadly.
Second, trust and confidence are fragile commodities, even in the best of times. Vaccination programs for Covid-19 are rolling out in an environment where individuals and communities are susceptible to misinformation, prone to overreact to news, and easily scared. Confidence could evaporate overnight simply due to:
Internationally, vaccines have become a foreign-policy tool. Some countries are receiving vaccines from China, Russia and the US through preferential commercial access, outright donations or strings-attached arrangements (“vaccine diplomacy”). These countries may struggle to convince their citizens that the vaccines they get are the best available and were obtained freely, instead of second-best options accepted under duress or in desperation. Complicating the political economy of vaccines further is the unfair global intellectual property regime that has led many people to distrust the products of “greedy” highly profitable pharmaceutical companies.
Fourth, confidence could be low because people perceive that governments or companies cut corners to develop, approve and manufacture Covid-19 vaccines so quickly. Public-health officials and the media may not have offered explanations for how science, economics and politics enabled such speed without compromising quality or safety. The are many logical reasons behind the success: Because Covid-19 affected rich countries (unlike other infectious diseases such as malaria or tuberculosis, which mainly affect poor countries), much more money and political will were channelled into its research. Also, there are more capable scientists than ever before, boosting the global capacity for knowledge exchange (including sharing of viral genetic material) and collaboration built on decades of extensive research into coronaviruses and mRNA vaccines. The basic science research into coronaviruses and vaccines already took place precisely in preparation for a pandemic such as Covid-19.
It was also much easier to enlist volunteers for vaccine testing. Pfizer, Moderna and Johnson & Johnson recruited a total of 117,000 subjects over six months for three separate global trials. Compare that with the three trials for the one Ebola vaccine that involved only 12,000 subjects from 2015 to 2017. Fierce competition among pharmaceutical companies delivered several safe and effective vaccines in a short time.
Finally, governments guaranteed purchases of Covid-19 vaccines through a tool called advanced market commitments, which gave the pharmaceutical companies the confidence to invest more money into research and manufacturing capacity. The speed should be regarded more as an indication of the robustness of a global collaborative scientific process and the presence of adequate incentives and political will.
There are other systemic reasons for vaccine hesitancy:
Pragmatic, holistic and sustainable
Given this wide range of powerful tectonic forces that may drive vaccine hesitancy, governments must significantly enhance their efforts to bolster vaccine confidence. To do this, governments must deploy political will and skill alongside science and facts.
There are three over-arching strategies to achieve confidence in vaccination programs. First, governments must adopt a suite of solutions as there is no single remedy to hesitancy. Second, governments must take an all-of-society approach because they do not possess all the required skills, capacity and trusting relationships to increase people’s willingness to get their shots. Third, these efforts must be continuous over a long term because vaccine confidence is a moving goalpost, with ever-changing circumstances and levels of trust. In short, vaccine confidence efforts must be pragmatic, holistic and sustainable.
Understanding the vaccine-confidence continuum is crucial for developing a full suite of solutions to hesitancy. Those actively demanding Covid-19 vaccines stand at one end, while those actively hostile to them are at the other. People can be divided into three groups along that spectrum, each requiring different approaches:
This neat landscape is complicated by numerous factors contributing to vaccine hesitancy that vary across countries, age groups, education and income levels, and political and religious beliefs. Education to strengthen vaccine confidence must, therefore, be nuanced and targeted to specific types of doubters, while focusing on four main areas:
When delivering vaccine education, governments must operate on several organizing principles. First, information must be extremely easy to understand and delivered repeatedly. Second, the messenger is as important as the message, which is why trusted figures such as teachers or religious leaders are helpful. Three, governments must treat their citizens as adults with dignity and agency, instead of being judgmental or paternalistic.
But education alone is not enough, no matter how nuanced, targeted or sustainable. Governments must deploy solutions to the other issues described earlier, including the following any or all of these strategies:
Although vaccine confidence is usually an individual matter, with levels varying within local communities and even within the same household, there are two important international considerations that require collaboration in the global commons:
The third and final overarching strategy to combat vaccine hesitancy is straightforward: confidence-building efforts must be sustainable and pursued over the long term. Covid-19 vaccination programs will be around for a while. Governments may never be able to declare “mission accomplished”. This means that efforts to shore up vaccine confidence must be permanent.
Indeed, if confidence-building measures are done well for the Covid-19 vaccines, there will be positive spillovers for other vaccines, increased health and science literacy, and greater trust in governments.
Vaccine confidence is not the only challenge
Vaccine hesitancy is only one reason why people do not get vaccinated. Other important causes include the lack of access (logistical or financial), fear of authorities, the collective action of selfish persons waiting for herd immunity, and conscientious objections or protests against governments and societies because of perceptions of coercion or threat. These complex issues need separate solutions.
Vaccine confidence is achievable. Building it requires coalitions of the willing, led by governments that deploys political will and skill alongside science and facts. Pragmatic, holistic and sustainable solutions are crucial if nations are to build back better, fairer and healthier after the pandemic.
Khor Swee Kheng
Chatham House (The Royal Institute of International Affairs) and the United Nations University-International Institute for Global Health
Check out here for more research and analysis from Asian perspectives.